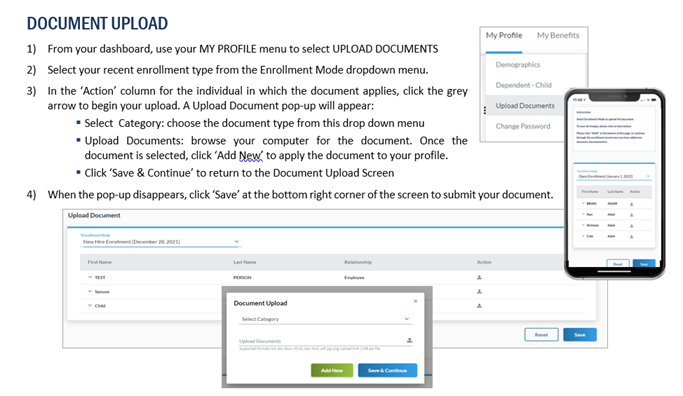
If you are waiving County medical or making changes to your covered dependents, employees must upload the associated valid documentation in order for benefits changes to be approved. Required documentation is the responsibility of the employee to upload into Benxcel's system within 31 days of the event date. See below infographic to ensure you upload and save your documentation correctly.
Once your documentation is uploaded, you will see it with the "pending" status. The documentation has been successfully uploaded and is waiting to be reviewed. No further action is required unless the documentation is rejected.
You will be notified via email and mail three times by Benxcel if you are outside this window and have not uploaded your required documentation. If you do not upload documentation within 31 days, you are at risk of having your Qualifying Event elections reversed.
Use the panels above to review each Qualifying Event and see the required documentation.