Benefits Enrollment and Qualifying Events
The County utilizes the Benxcel web interface for all benefits enrollments and demographic information. Benxcel is your one-stop-shop to update your address, process a Qualifying Event, or upload dependent documentation.
Aside from Open Enrollment, the only time you can make changes to specific benefit elections is when you experience a Qualifying Event (QE). Any changes you make must be consistent with the change in status occurring. You have 31 days from the event date to make any changes and to upload any required documentation needed.
When processing benefits changes for a Qualifying Event, it is important to know:
- Event Date
- Coverage Effective Date
- Required Documentation for the event
Please see the sections below for a list of common qualifying events and event details. Watch the tutorial video on How to Initiate a Qualifying Event in BenXcel. After completing your qualifying event, review and save a copy of your Confirmation Statement.
Qualifying Events Information
BenXcel Single sign on access will log you in to BenXcel.net when you are logged on to the County’s network. Click this link to utilize BenXcel Single sign on access. When you are not connected to the County’s network, you can continue to login using your BenXcel user name and password. Review instructions below to see how to do so.
-
USER ID: First letter of first name, full last name, entire DOB
-
EX: Judy Smith-Doe DOB: 01/25/1973
-
USER ID: jsmithdoe01251973
-
- PASSWORD:
- Current Employees: Your password will be whatever you reset it to be last Open Enrollment. If you cannot remember your password and need a reset you can either click Forgot Password under the login box or call BCC at 1-800-685-6100.
- New Hires: Full Last name, first letter of first name, last four of Social Security Number (SSN).
-
Example: Judy Smith-Doe SSN: 123-45-6789
PASSWORD: smithdoej6789
- Company Name: SLO
If you are having system issues or have forgotten your username and/or password, you must call BCC at 1-800-685-6100 for assistance. If you enter wrong username or password more than 5 times, you will be locked out and will need to call BCC.
While in BenXcel, you can review your Confirmation Statement at anytime. Find steps on how to view your Confirmation Statement here.
If you're a new employee looking to make your benefits elections, please login using the instructions above. Take a moment to review the current Employee Benefits Brochure under General Resources, and read the Compare Medical Plans webpage to better understand your options before enrolling. Click the thumbnail below to watch the New Hire enrollment tutorial.
If you have questions or difficulties enrolling, reach out to your Payroll Coordinator for assistance. You have 30 days from your hire date to make any changes to your new hire enrollment. Coverage begins the first of the month after the employee hire date.
BenXcel Qualifying Event Name: Birth of a Baby, Adoption of a Child, or New Legal Guardianship
| Qualifying Event Date | Coverage Effective Date | Required Documentation |
|---|---|---|
| Date of Birth, Adoption, or Legal Guardianship |
Date of Birth (medical only) 1st of month following Event Date (all other coverages) |
|
While coverage is not active until the first of the following month, newborn babies are typically covered under the mother's insurance for the first month of birth. When handling billing, you may need to confirm that charges will billed under the mother's name.
Permitted Benefits Changes
| Benefit Type | Permitted Change |
|---|---|
| Medical Plan |
|
| Dental Plan |
|
| Vision Plan |
|
| Tax Savings Accounts |
|
| Voluntary Voya and Aflac Plans |
|
BenXcel Qualifying Event Name: Marriage or Domestic Partnership*
*Domestic Partnership - please see important IRS information below Permitted Benefits Changes
| Qualifying Event Date | Coverage Effective Date | Required Documentation |
|---|---|---|
| Date of Marriage or Partnership |
1st of month following Event Date (all other coverages) |
|
***It is the employee's responsibility to upload required documentation into BenXcel AND to provide San Luis Obispo County Pension Trust (SLOCPT) a copy of the marriage certificate. Contact SLOCPT at (805) 781-5465 or email [email protected].
Permitted Benefits Changes
| Benefit Type | Permitted Change |
|---|---|
| Medical Plan |
|
| Dental Plan |
|
| Vision Plan |
|
| Tax Savings Accounts |
|
| Voluntary Voya and Aflac Plans |
|
For employees who enroll their domestic partners in health plans here is additional information:
- Employees cannot pay their portion of domestic partner premiums on pre-tax basis.
- The additional premium to cover the domestic partner must be paid on a post-tax basis.
- Answers to Frequently Asked questiosn for Registered Domestic Partners and Individual Civil Unions | Internal Revenue Service
BenXcel Qualifying Event Name: Divorce
| Qualifying Event Date | Coverage Effective Date | Required Documentation |
|---|---|---|
|
Date of Divorce |
Benefits for spouse and stepchildren will terminate at the end of divorce month |
|
NOTE: This is a mandatory event to remove spouse and stepchildren from all enrolled plans
- Former spouses and stepchildren are not eligible for the County's insurance plans.
- For late notifications, employees are personally responsible for claims incurred by ineligible dependents and premium costs incurred after coverage effective date.
Permitted Benefits Changes
| Benefit Type | Permitted Change |
|---|---|
| Medical Plan |
|
| Dental Plan |
|
| Vision Plan |
|
| Tax Savings Accounts |
|
| Voluntary Voya and Aflac Plans |
|
BenXcel Qualifying Event Name:
- Drop Self and Dependents from Medical due to New Eligibility for Other Group Coverage
- Select this option if you (the employee) are dropping County medical coverage due to having other group coverage.
- Drop Dependents from Medical, Dental, or Vision due to New Eligibility for Other Group Coverage
- Select this option if you (the employee) are remaining on County medical coverage, but your dependent(s) will be dropped and move to the new other group coverage.
| Qualifying Event Date | Coverage Effective Date | Required Documentation |
|---|---|---|
|
Date Dependent(s) current coverage should terminate |
1st of month following event date |
|
- If you (the employee) are dropping your County medical coverage due to having other group coverage
- Choose Event #4 in BenXcel: Drop Self and Dependents from Medical due to New Eligibility for Other Group Coverage
- If you (the employee) are remaining on County medical coverage, but your dependents will move to the new other group coverage
- Choose Event #5 in BenXcel: Drop Dependents from Medical, Dental, or Vision due to New Eligibility for Other Group Coverage
Permitted Benefits Changes
| Benefit Type | Permitted Change |
|---|---|
| Medical Plan |
|
| Dental Plan |
|
| Vision Plan |
|
| Tax Savings Accounts |
|
| Voluntary Voya and Aflac Plans |
|
BenXcel Qualifying Event Name: Add Self and Dependents to Medical, Dental, and/or Vision due to Loss of Other Group Coverage
| Qualifying Event Date | Coverage Effective Date | Required Documentation |
|---|---|---|
|
Date Other Group Coverage Ended |
1st of month following event date |
|
Permitted Benefits Changes
| Benefit Type | Permitted Change |
|---|---|
| Medical Plan |
|
| Dental Plan |
|
| Vision Plan |
|
| Tax Savings Accounts |
|
| Voluntary Voya and Aflac Plans |
|
BenXcel Qualifying Event Name: Phone Number, Address, or Email Change
You must update your phone number, address, and/or email both with SAP and BenXcel. To update your demographic information in BenXcel, you will need to initiate the above Qualifying Event.
- Login to BenXcel
- Go to "Initiate a Qualifying Event"
- Select "8. Phone Number, Address, or Email Change"
- Enter in today's date for the event date
- Update the necessary demographic information
BenXcel Qualifying Event Name: HSA Contribution Update
If you are on the High Deductible Health Plan (HDHP), you may be eligible for a Health Savings Account (HSA). All County employees are eligible to receive an employer contribution to the HSA, in addition, to electing an employee contribution amount.
Employees do not have to contribute to the HSA to receive the employer contribution. The employee contribution is voluntary. You may change your employee HSA contribution amount anytime throughout the year, by initiating the corresponding qualifying event in BenXcel.
- Login to BenXcel
- Go to "Initiate a Qualifying Event"
- Select "9. HSA Contribution Update"
- Enter in today's day for the event date
- Update the contribution amount
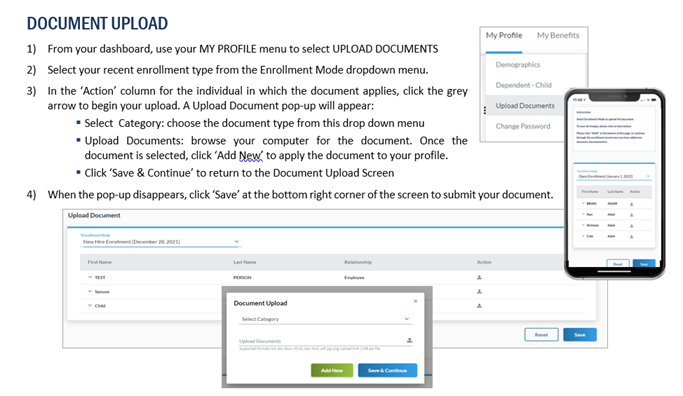
If you are waiving County medical or making changes to your covered dependents, employees must upload the associated valid documentation in order for benefits changes to be approved. Required documentation is the responsibility of the employee to upload into Benxcel's system within 31 days of the event date. See below infographic to ensure you upload and save your documentation correctly.
Once your documentation is uploaded, you will see it with the "pending" status. The documentation has been successfully uploaded and is waiting to be reviewed. No further action is required unless the documentation is rejected.
You will be notified via email and mail three times by Benxcel if you are outside this window and have not uploaded your required documentation. If you do not upload documentation within 31 days, you are at risk of having your Qualifying Event elections reversed.
Use the panels above to review each Qualifying Event and see the required documentation.
For each Qualifying Event, there is required documentation. Please review the above panels to determine what documentation you need and how to upload it into BenXcel. If you need additional assistance obtaining the required documentation, you can use the resources below:
Birth Certificate for Newborns, Stepchildren, and Legal Guardianship
- County office that issued original birth certificate
- Hospital in which child was born
- U.S. Department of State (for children born outside of the U.S)
- Social Security Administration
- Vitalchek.com
Adoption Paperwork
- State agency that issued final adoption papers
- Adoption agency that issued placement papers
- Social Security Administration
Marriage Certificate, Certificate of Domestic Partnership, Divorce Decree, and Termination of Domestic Partnership
- County office that issued original marriage certificate or certificate of domestic partnership
- Vitalchek.com
- sos.ca.gov/registries/domestic-partners-registry
Proof of Other Group Coverage/Proof of Loss of Other Group Coverage
- Contact new/old employer for paperwork
- Employer can provide a hire letter stating benefits coverage (with dependents listed)
- Employer can provide a letter stating benefits termination (with dependents listed)
- Request a "Letter of Credible Coverage" or a "Confirmation of Benefits" letter
- Submitted proof of health coverage must reflect active or recent coverage within the last year (2025 or 2026). Documentation from earlier years, such as 2020, will not be accepted.

.png)
